modern male-to-female sex reassignment surgery
modern male-to-female sex reassignment surgery
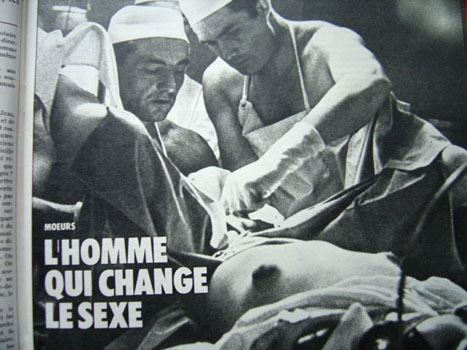
Photos of Dr. Burou
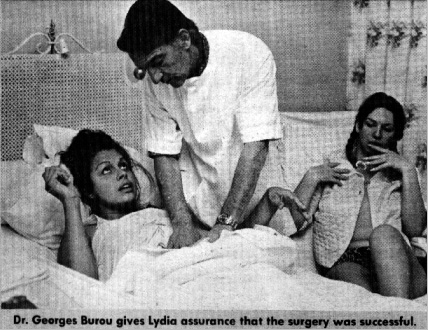
Dr. Burou with his wife Lisa
[ Many thanks to Pascale from France for finding and sending these photos. ]
PROCEEDINGS
OF THE SECOND INTERDISCIPLINARY SYMPOSIUM
ON GENDER DYSPHORIA SYMDROME
[from p. 247]
The Symposium
The Interdisciplinary Symposium on Gender Dysphoria Syndrome was held at the Stanford University School of Medicine, February 2-4, 1973.
The purpose of the meeting was to provide a forum for the exchange of scientific information about the patient who desires and is considered for gender re-identification.
The symposium was sponsored by the Divisions of Urology and Plastic and Reconstructive Surgery at the Stanford School of Medicine. Its principal architect and chairman was Donald R. Laub, M.D., Chief of the Division of Plastic and Reconstructive Surgery.
Participants and contributors included 105 representatives of the major teams and private practitioners concerned with the diagnosis, evalutaion, and social adjustment of the gender dysphoric patient. The group included psychiatrists, surgeons, obstetricians and gynecologists, attorneys, psychologists, sociologists, and experts in epidemiologic and health services research.
In addition to the United States, numerous representatives from Canada, Mexico, England, Morocco and Australia were present.
Male to Female Transformation
Georges Burou, M.D.*
Dr. Burou is a gynecologist from Morocco who had previous experience making a neo-vagina in cases of vaginal atresia. He treated a male patient who insisted upon sex reassignment surgery and went into this field. When Dr. Burou created the operation, he was totally unaware of previous such work in the world. He thought at the time that the best thing to do was to utilize the live graft which can be made from the penile skin when properly dissected. this is what he is going to describe now. This is the first report on this new technique.
Dr. Burou want to thank very much many American physicians who supported him in this work, referring many American patients, and who have been extremely helpful in corresponding with him.
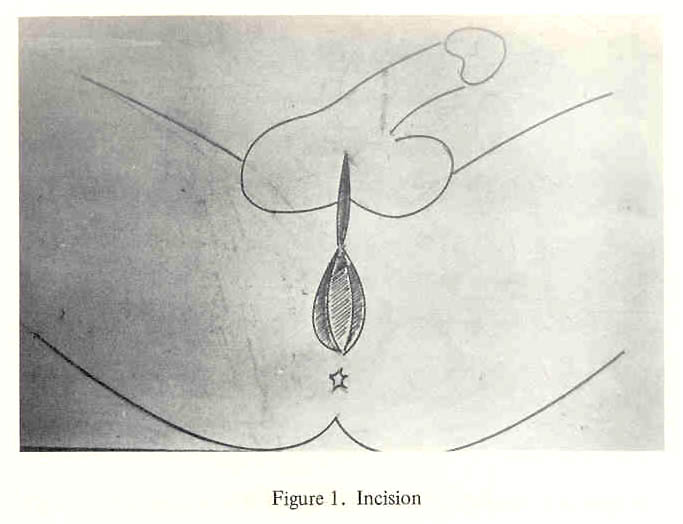
The entire surgical operation is done in one stage, consisting of two successive steps. All of the patients who under go surgery have been prepared, undergo psychiatric care, on hormones, and made quite feminine. The first step is made on a very narrow surgical field and the goal of this first step is to create a space between the rectum and the prostate. The fist incision is made posteriorly between the anal area and the scrotal ridge. This first part is extremely important, because you can determine at any time by intrarectal inspection that there is no lesion to the rectal wall. This is very important to avoid any further complications during the dissection in the rectum in the prerectal space. Figure 1 shows the first incision going from the anal area through the ridge of the scrotum. On the left of the figure is the first dissection of the bulb and both corpora cavernosa. The cleavage between the rectum and the prostate is made by cutting all the ligaments between the bulb and the rectum. Then Dr. Burou positions the cleavage with his finger in the natural space which is between the rectal wall and the prostate. The cleavage is done when you admit easily two fingers of a vaginal retractor. One can meet at the end of this new space a natural formation which makes you feel that you are really meeting the natural vaginal cul-de-sac, Douglas space. The first step is over.
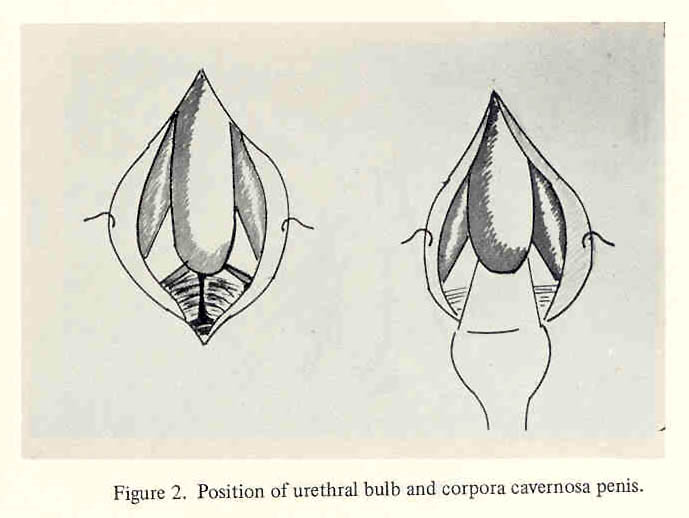
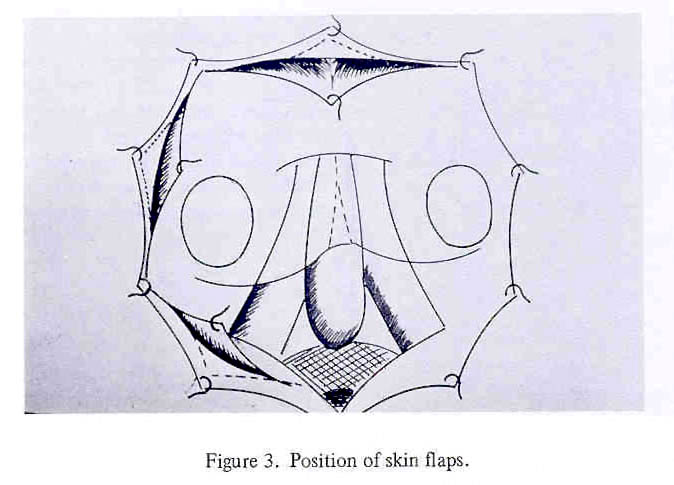
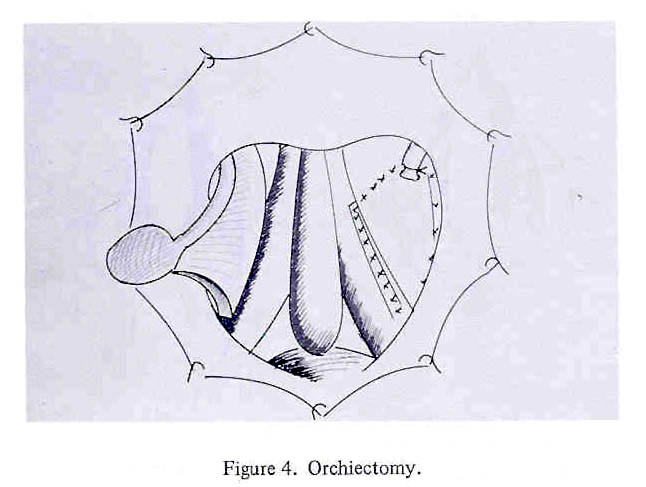
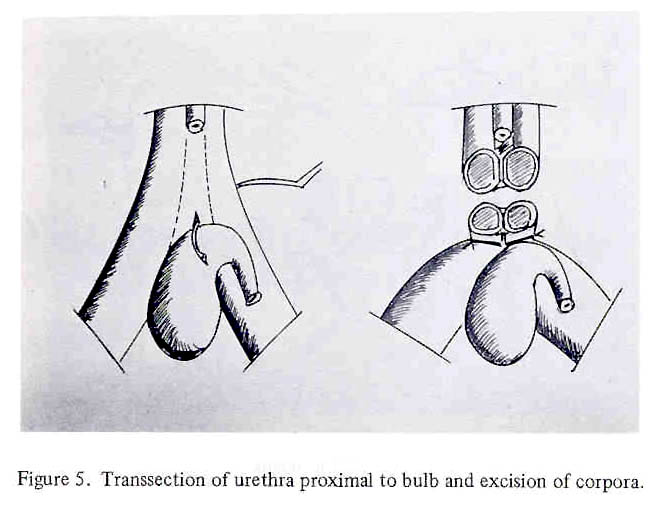
The first step is in fact the most important and most dangerous. The second one is relatively easy. One enlarges the surgical field in the most usual way, taking all the usual precautions. The initial incision is now prolonged under the scrotum to the root of the penis. The surgical field is widened by retracting and widely exposing the scrotal skin on both sides. On the neocolporrhaphy we have both the corpora cavernosa, spongiosa, and the two testes. The testes and its beaker will be cleaved by cleavage of the fiberous tunica. Figure 2 shows that the high testes has been dissected through the fat pad attached to it. It is separated on the inside from the corpora cavernosa, and it is also freed from the lateral wall. Once the testes and all the surrounding pedicle have been freed, the spermatic chord is cut and ligated, as can be seen in Figure 3. Removing the section of the testes and all the mass surrounding it, requires very careful hemostatis and the right sectioning of the bulb, corresponding to the future urethra. The right of Figure 3 shows where both corpora cavernosa will be sutured; the needle is visible. On the right the corpora cavernosa is shown firmly sutured with the future urethra pending on the right. Above are the erectile bodies of the penis. The left side of Figure 4 shows the erectile bodies being pushed out and dissected from the penile skin. Figure 5 shows that practically all of the skin of the penis now has been completely freed from the erectile bodies. Figure 6 shows the complete dissection of the penile skin; you even keep the foreskin when available. It is at this stage that the end of the penile skin is being sutured and closed. This will constitute later on the neovagina.
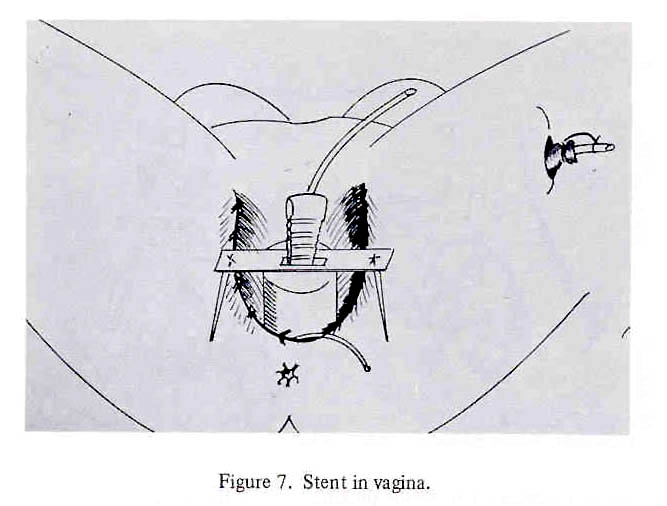
Figure 6 shows the neovagina quite ready to be inserted in the prerectal space which was created. On the lower abdominal skin is a slight skin slit which will allow the future urethra to be passed through. The figure also shows an important feature coming through the skin near the anal area - two threads which are being inserted on the anterior ani muscle. These two threads will serve to support a bougie of Eggar, a prosthetic instrument known in obstetrics. This bougie of Eggar will be placed in the neovagina to provide support. Figure 7 shows a drain with aspiration which is being placed in the posterior commissure. The bougie of Eggar is in place, and the two threads coming from the skin are tightening very closely and very firmly that bougie of Eggar into the neovagina. It is easy to regulate or test the firmness and tension on the two threads. At this stage excess skin flap must be removed in order to obtain a good appearance. Figure 7 shows the exit of the levator cannula with catheter. There is no skin suture. The urethra is being sutured on the catheter, about .5 cm from the skin. Some kind of retraction must always be foreseen. Figure 7 also shows the drainage at the posterior commissure.
Eight days after surgery, the bougie of Eggar was maintained for 48 hours. The aspiration is also removed after 48 hours. The urethral catheter is maintained for four days. The management of the new vagina is being made by frequent and daily introductions of small vaginal retractors. In the next few days permeability of the urethra must also be maintained by daily introduction of the catheter and making sure that there is no stenosis that it is completely patent. With the catheter, the urethra is immediately introduced at the appropriate place during the final step.
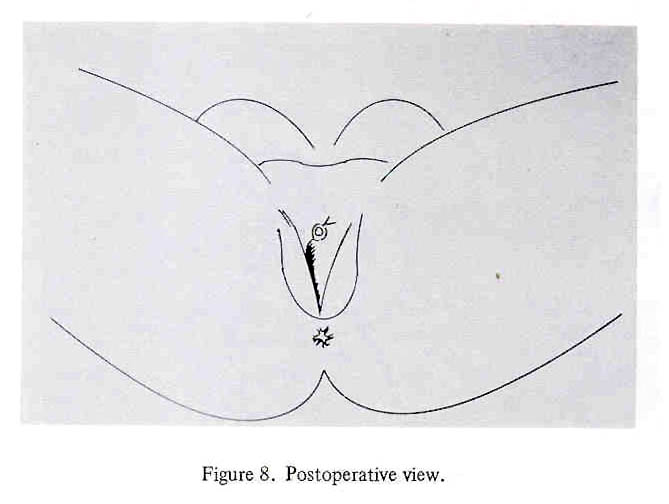
[Note: Figure 8 shows the final postoperative view.]
________________
*This report is a translation of Dr. Burou's remarks
LynnConway.com > TS Information > Transsexualism > Sex Reassignment Surgery > Burou